Common drugs tied to increased risk of cognitive decline
From the September 2, 2020 American Academy of Neurology Press Release
https://www.aan.com/PressRoom/Home/PressRelease/3818
MINNEAPOLIS – A class of drugs used for many conditions, including allergies, colds, high blood pressure and depression, may be associated with an increased risk of developing mild thinking and memory problems, particularly in people who have genetic risk factors for Alzheimer’s disease or markers of this condition, according to a study published in the September 2, 2020, online issue of Neurology®, the medical journal of the American Academy of Neurology. These types of drugs, called anticholinergic drugs, are used for motion sickness, urinary incontinence, overactive bladder, Parkinson’s disease and high blood pressure. There are approximately 100 such drugs in widespread use, with some requiring a prescription and many others that may be purchased over-the-counter. The study found that cognitively normal people taking at least one anticholinergic drug were 47% more likely to develop mild cognitive impairment, which can be a precursor to dementia, over the next decade than people who were not taking such drugs.


Of the 230 people who were taking anticholinergic drugs, 117 people, or 51%, later developed mild cognitive impairment, compared to 192 people, or 42%, of the 458 people who were not taking the drugs. After adjusting for depression, number of medications being taken, and history of cardiac problems, individuals taking at least one anticholinergic drug had a 47% increased risk for developing mild cognitive impairment. Furthermore, those with higher overall exposure to anticholinergic drugs had additional increased risk. Researchers also looked at whether people had had biomarkers for Alzheimer’s disease in their cerebrospinal fluid or had genetic risk factors for Alzheimer’s disease.
Read the entire article at https://www.aan.com/PressRoom/Home/PressRelease/3818
Children growing up in low greenery areas at risk of losing IQ points
From the 26 August 2020 article by Bob Yirka, Medical Press

“A team of researchers affiliated with multiple institutions in Belgium has found that children who grow up in areas with little greenery are at risk of scoring lower on IQ tests. In their paper posted on the open access site PLOS Medicine, the group describes their study of children’s IQ and the amount of greenery where they were growing up, and what they found.”
11 foods that lower cholesterol
From the 2019 article at Harvard Health
“
Changing what foods you eat can lower your cholesterol and improve the armada of fats floating through your bloodstream. Adding foods that lower LDL, the harmful cholesterol-carrying particle that contributes to artery-clogging atherosclerosis, is the best way to achieve a low cholesterol diet.

Add these foods to lower LDL cholesterol
Different foods lower cholesterol in various ways. Some deliver soluble fiber, which binds cholesterol and its precursors in the digestive system and drags them out of the body before they get into circulation. Some give you polyunsaturated fats, which directly lower LDL. And some contain plant sterols and stanols, which block the body from absorbing cholesterol.”
Click here to see the list which includes oats, beans, nuts, and vegetable oils.
Is your pet’s food making you sick? Study finds many don’t know the risk
From the August 19, 2020 article by Brian Wallhemer at MedicalXpress
“many Americans don’t wash their hands after feeding or playing with their cats and dogs and aren’t aware of the risk of contracting a foodborne illness from those activities.”

“Some tips to keep pet owners from getting foodborne illness include:
–Wash hands with soap and water after preparing food for pets, petting or playing with pets, and before preparing food for people.
–Avoid feeding pets raw meat.
–Handle and store pet food carefully to avoid cross-contamination.
–Keep up with pet food recalls and keep records of pet food lot numbers and other information for potential tracking.”
Honey found to be a better treatment for upper respiratory tract infections than traditional remedies
From the August 29, 2020 article by Bob Yirka at MedicalXpress

“A trio of researchers at Oxford University has found that honey is a better treatment for upper respiratory tract infections (URTIs) than traditional remedies. In their paper published in BMJ Evidence-based Medicine, Hibatullah Abuelgasim, Charlotte Albury, and Joseph Lee describe their study of the results of multiple clinical trials that involved testing of treatments for upper respiratory tract infections (URTIs) and what they learned from the data.”
“The researchers note that the reason honey works as a treatment for URTIs is because it contains hydrogen peroxide—a known bacteria killer—which also makes it useful as a topical treatment for cuts and scrapes. Honey is also of the right consistency—its thickness works to coat the mouth and throat, soothing irritation.”
The article also states honey is better than antibiotics.
How much honey? Unclear at this time. According to the article…
“Finally, we could not explore the effectiveness of different types or doses of honey due to lack of data.”
Examine.com – Science-based nutrition & supplement information

Examine.com simplifies nutrition and supplementation — through meticulous analysis of the latest scientific research — to help answer your questions on how to be healthier.
Go here for list of supplements, by name and by use (as gut health)
Go here for Top nutrition and supplement articles
Go here for Guides (sorry about that ad, $99.00 for all 17 guides – Yikes!)
This Web site was recommended to me by a physician.
Fighting injustice can trigger trauma — we need to learn how to process it and take healing action
From the August 28, 2020 blog item at Waging Nonviolence by Kazu Gaga
“Perhaps you have noticed signs of trauma playing out in your own life, in your relationships and in your household. Common responses to trauma can include anxiety, short tempers, hyper-vigilance, withdrawal, fatigue, cynicism, lack of empathy and restlessness, among countless others.”
“When trauma is triggered, we lack the ability to take in new information, to be creative, consider different perspectives or think about long-term consequences.”
How do we engage? Study trauma, move through trauma, slow down, and open up.
Read the entire article here.

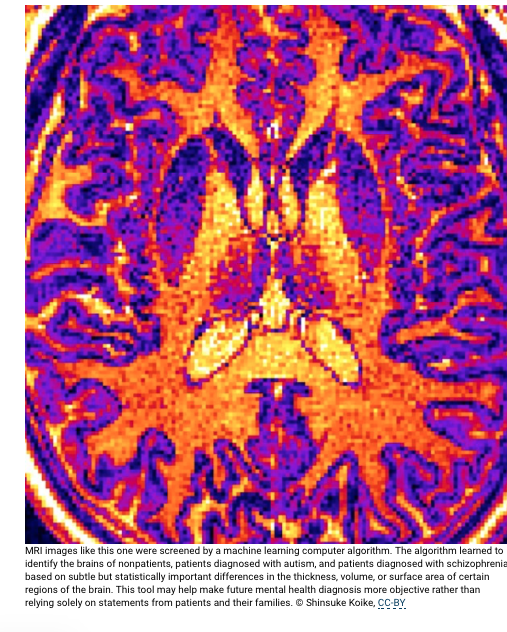
Future mental health care may include diagnosis via brain scan and computer algorithm
Computer IDs differences in brains of patients with schizophrenia or autism
From the August 20, 2020 news release from the University of Tokyo
“
A multidisciplinary team of medical and machine learning experts trained their computer algorithm using MRI (magnetic resonance imaging) brain scans of 206 Japanese adults, a combination of patients already diagnosed with autism spectrum disorder or schizophrenia, individuals considered high risk for schizophrenia and those who experienced their first instance of psychosis, as well as neurotypical people with no mental health concerns. All of the volunteers with autism were men, but there was a roughly equal number of male and female volunteers in the other groups.
Machine learning uses statistics to find patterns in large amounts of data. These programs find similarities within groups and differences between groups that occur too often to be easily dismissed as coincidence. This study used six different algorithms to distinguish between the different MRI images of the patient groups.
The algorithm used in this study learned to associate different psychiatric diagnoses with variations in the thickness, surface area or volume of areas of the brain in MRI images. It is not yet known why any physical difference in the brain is often found with a specific mental health condition.”
Patients taking opioids produce antibodies that may hinder anti-opioid vaccine
From the August 17, 2020 news release at the University of Wisconsin-Madison
“University of Wisconsin–Madison scientists have discovered that a majority of people they tested who were taking opioid painkillers for chronic back pain produced antibodies against the drugs that may contribute to some of the negative side effects of long-term opioid use.”
…

…”For decades, researchers have understood that the immune system can produce antibodies against psychoactive drugs under the right conditions. While the chemicals themselves are too small for the immune system to recognize, they can permanently bind to large proteins in the blood, which can then trigger an immune response.”…
Read the entire article here
…”If a vaccine can produce antibodies capable of neutralizing the drugs, it could help people combat addiction by reducing the pleasurable feelings the drugs produce in the brain. Past trials of vaccines against nicotine or cocaine have had limited success, in part because of individual differences in how the immune system produces antibodies.”…
——————–
Related article & 3 minute video
Negative side effects of opioids could be coming from users’ own immune systems (video) (American Chemical Society, August 17, 2020)
This video, in 3 minutes, summarizes the University of Madison-Wisconsin article
Looking for Biological Product Information? Try the FDA’s Purple Book
From the February 20 article at Regulatory Focus News
“Regulatory Focus: FDA Launches Searchable Purple Book. “The US Food and Drug Administration (FDA) on Monday unveiled the first version of its searchable online database of biological product** information, known as the Purple Book. Building off the previous PDF lists of biological products, the database now allows for easier searches and includes information on product names (proprietary and proper), the type of biologics license application (BLA) that was submitted, strength of the biologic, dosage form, product presentation, license status, BLA number and approval date.” I didn’t know how a “biological product” was defined. I got educated via this FDA PDF.“
Click Image for Larger Version
***What is a biological product?
Biological products include a wide range of products such as vaccines, blood and blood components, allergenics, somatic cells, gene therapy, tissues, and recombinant therapeutic proteins. Biologics can be composed of sugars, proteins, or nucleic acids or complex combinations of these substances, or may be living entities such as cells and tissues. Biologics are isolated from a variety of natural sources – human, animal, or microorganism – and may be produced by biotechnology methods and other cutting-edge technologies. Gene-based and cellular biologics, for example, often are at the forefront of biomedical research, and may be used to treat a variety of medical conditions for which no other treatments are available.
Yoga Shown to Improve Anxiety, Study Finds
From the August 12, 2020 NYU Langone Health NewsHub

“Yoga improves symptoms of generalized anxiety disorder, a condition with chronic nervousness and worry, suggesting the popular practice may be helpful in treating anxiety in some people.
Led by researchers at NYU Grossman School of Medicine, a new study found that yoga was significantly more effective for generalized anxiety disorder than standard education on stress management, but not as effective as cognitive behavioral therapy (CBT), the gold standard form of structured talk therapy that helps patients identify negative thinking for better responses to challenges.”
Read the entire article here.
Aging memories may not be ‘worse,’ just ‘different’
From The August 20, 2020 news release of the Washington University in St. Louis

Excerpts
“Memory is the first thing to go.”
Everyone has heard it, and decades of research studies seem to confirm it: While it may not always be the first sign of aging, some faculties, including memory, do get worse as people age.
It may not be that straightforward…..
….Much of the activity he was interested in is in an area of the brain referred to as the posterior medial network — which includes regions in the midline and toward the backside of the brain. In addition to memory, these areas are heavily involved in representing context and situational awareness. Some of those areas showed decreased activity in the older adults.
“We do think the differences are memory-related,” Reagh said. At the boundaries, they saw differences in the levels of activity in the hippocampus that was related to memory in a different measurement — “story memory,” he called it.
“There might be a broad sense in which the hippocampus’s response to event boundaries predicts how well you are able to parse and remember stories and complex narratives,” no matter one’s age, Reagh said.
But for older adults, closer to the front of the brain, particularly the medial prefrontal cortex, things were looking up.
Activity in that area of the brain was ramped up in older adults. This area is implicated in broad, schematic knowledge — what it’s like to go to a grocery store as opposed to a particular grocery store.
“What might be happening is as older adults lose some responsiveness in posterior parts of the brain, they may be shifting away from the more detailed contextual information,” Reagh said. But as activity levels heighten in the anterior portions, “things might become more schematic. More ‘gist-like.’”
In practice, this might mean that a 20-year-old noting an event boundary in a movie might be more focused on the specifics — what specific room are the characters in? What is the exact content of the conversation? An older viewer might be paying more attention to the broader picture — What kind of room are the characters in? Have the characters transitioned from a formal dinner setting to a more relaxed, after-dinner location? Did a loud, tense conversation resolve into a friendly one?
“Older adults might be representing events in different ways, and transitions might be picked up differently than, say, a 20-year-old,” Reagh said.
“An interesting conclusion one could draw is maybe healthy older adults aren’t ‘missing the picture.’ It’s not that the info isn’t getting in, it’s just it’s getting in differently.”
New study documents increasing frequency, cost, and severity of gunshot wounds that require surgical intervention
From the August 10 2020 news release from the American College of Surgeons
Researchers hope findings drive changes to address violence and hospital costs
“The rise in firearm violence has coincided with an increase in the severity of injuries firearms inflict as well as the cost of operations to treat those injuries; policy makers must be more aggressive in addressing violence to curb these trends, researchers report in a large national study of gunshot wounds that appears as an “article in press” on the Journal of the American College of Surgeons website ahead of print.

“Taken together, our findings suggest that gun violence has increased in numbers, at least for the sector that meets surgical criteria, and that these injuries result in a substantial financial burden in addition to the obvious psychosocial burden and other downstream effects..”
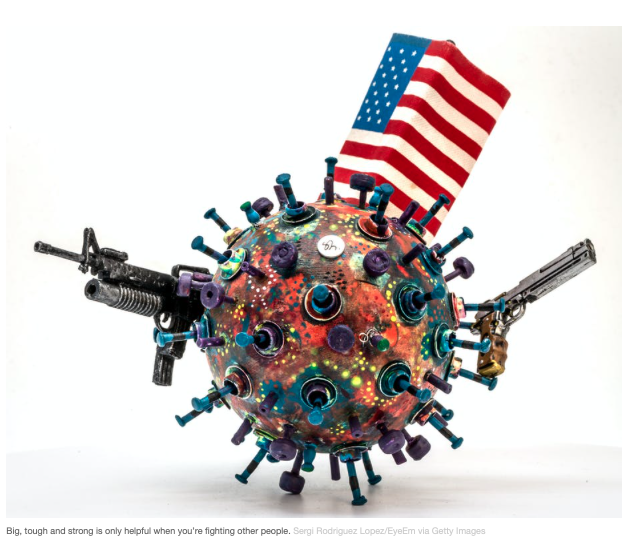
Why Coronavirus is More Dangerous than the Flu

There are many myths surrounding coronavirus.

One myth states flu kills more people than the coronavirus. This may be true for some countries. However in the US
— 62,000 people died from the flu between October 1 and April 4, that means the US had an average of about 331 flu deaths a day
— February 6 through April 30, an average of more than 739 coronavirus deaths per day
–Different times frame, but if we get the second wave of COVID-19 infections, we could get continue to get more coronavirus deaths than flu deaths even during the peak of flu season (December-February).
Other myth busters about the danger of the coronavirus
—Coronavirus is much more contagious than the flu
— Research shows a person with the flu infects an average of about 1.28 other people
–a person with the COVID-19 virus infects an average of about 2 to 3 other people. This includes people who show no symptoms.
—Coronavirus can be spread for many days without symptoms
— People show flu symptoms often within two days according to the CDC
— People show COVID-19 symptoms within four or five days after exposure,” according to Harvard Medical Schoo, if you’ve been exposed to the coronavirus And many people
never show symptoms, but can still spread the virus.
—You can get a flu vaccine but not a coronavirus vaccine
The earliest a COVID-19 vaccine will be available will be December of this year
Soures/References
—Critics said the flu kills more than coronavirus. Why that’s not a fair comparison — and now, it’s not even true (CNN)
—Coronavirus disease (COVID-19) advice for the public: Mythbusters (WHO)
—If you’ve been exposed to the coronavirus (Harvard Medical Letter)
—Get the Facts About Coronavirus (CDC)
—Debunking COVID-19 (coronavirus) myths (Mayo Clinic)
—7 Dangerous Myths About The COVID-19 Coronavirus Pandemic
—21 Myths About Coronavirus You Need to Stop Believing Now
And for anyone trying to convince anyone that this virus is real and precautions are necessary, here is a good read.
I’ve been talking to conspiracy theorists for 20 years – here are my six rules of engagement
Great closing thought…
“6. Finally, be realistic
There is, of course, no guarantee that this advice will be effective. There are no incontestable arguments or fail-proof strategies that will always convert a conspiracy theorist to scepticism. Therefore, set realistic expectations. The aim of talking to conspiracy theorists is not to convert them, but to sow doubt about an argument, and hopefully enable them to gradually build up resistance to its seductive appeal.”
Sex redefined : Nature News & Comment
The idea of two sexes is simplistic
Biologists now think there is a wider spectrum than that

From the February 18, 2015 Nature News Feature
““The main problem with a strong dichotomy is that there are intermediate cases that push the limits and ask us to figure out exactly where the dividing line is between males and females,” says Arthur Arnold at the University of California, Los Angeles, who studies biological sex differences. “And that’s often a very difficult problem, because sex can be defined a number of ways.”
The article goes on to explain DSDs (Differences/Disorders in Sexual Development) both in and out of the womb.
Read the entire news item here
Study looks at why people may feel more helpless in stressful situations than others
Scientists have identified a list of brain areas that might have a critical role to play in stress-induced depression
From the March 30, 2019 EurekAlert

“Certain patterns were revealed in the stressed brain and the scientists identified a list of brain areas that might have a critical role to play in stress-induced depression. Looking at these brain activities the study, published in Frontiers in Neural Circuits, opens up possibilities for identifying new targets for the treatment of depression.
They explain that with the exception of a few brain areas, “mice showing ‘helpless’ behavior had an overall brain-wide reduction in the level of neuronal activation compared with mice showing ‘resilient’ behavior.”
“In addition, the helpless mice showed a strong trend of having higher similarity in whole-brain activity profile among individuals, suggesting that helplessness is represented by a more stereotypic brain-wide activation pattern,” explained the authors of the study.”
Read the entire news release at https://www.eurekalert.org/pub_releases/2016-03/f-sla033016.php
Why synthetic drugs are as scary as you think (video)
From the March 16, 2016 American Chemical Society news release
WASHINGTON, March 29, 2016 — Synthetic drugs such as “bath salts,” “K2” or “Spice” have made unsettling headlines lately, with reports of violent, erratic behavior and deaths after people have used the substances. Why are these synthesized drugs so dangerous, and why aren’t there more regulations? In this week’s Reactions, we answer these questions by examining the chemistry of two kinds of synthetic drugs: bath salts and synthetic marijuana. Check out the video here: https://youtu.be/83gIiBD365E.

Plates, cups and takeaway containers shape what (and how) we eat

From the June 2, 2020 article at The Conversation
“Home cooks have been trying out their skills during isolation. But the way food tastes depends on more than your ability to follow a recipe.
Our surroundings, the people we share food with and the design of our tableware – our cups, bowls and plates, cutlery and containers – affect the way we experience food.
Read more: Should we eat breakfast like a king, lunch like a prince, and dinner like a pauper?
For example, eating from a heavier bowl can make you feel food is more filling and tastes better than eating from a lighter one.
Contrast this with fast food, which is most commonly served in lightweight disposable containers, which encourages fast eating, underestimating how much food you’re eating, and has even been linked to becoming impatient.
These are just some examples of the vital, but largely unconscious, relationship between the design of our tableware – including size, shape, weight and colour – and how we eat.”
Read the entire article for how the following affect the experience of eating
— color of your crockery (as cups and plates)
for example, colored crockery tend to make food taste sweeter!
–plastics
–aesthetics
The fascinating history of clinical trials

From the June 3, 2020 article at The Conversation
“Clinical trials are under way around the world, including in Australia, testing COVID-19 vaccines and treatments.
These clinical trials largely fall into two groups. With observational studies, researchers follow a group of people to see what happens to them. With experimental studies, people are assigned to treatments, then followed.
These study designs have come about from centuries of people trying out different ways of treating people.
Here are some of the key moments in the history of clinical trials that led to the type of trials we see today for COVID-19.”
Continue reading the article for examples as ginseng in China, rhubarb in 18th century England, Early 20th-century randomised trial, and tuberculosis and the randomised controlled trial
Additional resources and reading
—Randomised control trials: what makes them the gold standard in medical research?
–From the research lab to your doctor’s office – here’s what happens in phase 1, 2, 3 drug trials
— Health Check: can vitamins supplement a poor diet?
—ClinicalTrials.gov – a searchable database of privately and publicly funded clinical studies conducted around the world.
How psychedelic drug psilocybin works on brain

From the June 4, 2020 article at Johns Hopkins University Medicine
Research Story Tip:
Psychedelic Drug Psilocybin Tamps Down Brain’s Ego Center
Excerpt:
“Perhaps no region of the brain is more fittingly named than the claustrum, taken from the Latin word for “hidden or shut away.” The claustrum is an extremely thin sheet of neurons deep within the cortex, yet it reaches out to every other region of the brain. Its true purpose remains “hidden away” as well, with researchers speculating about many functions. For example, Francis Crick of DNA-discovery fame believed that the claustrum is the seat of consciousness, responsible for awareness and sense of self.”
What is known is that this region contains a large number of receptors targeted by psychedelic drugs such as LSD or psilocybin — the hallucinogenic chemical found in certain mushrooms. To see what happens in the claustrum when people are on psychedelics, Johns Hopkins Medicine researchers compared the brain scans of people after they took psilocybin with their scans after taking a placebo.
Their findings were published online on May 23, 2020, in the journal NeuroImage.
The scans after psilocybin use showed that the claustrum was less active, meaning the area of the brain believed responsible for setting attention and switching tasks is turned down when on the drug. The researchers say that this ties in with what people report as typical effects of psychedelic drugs, including feelings of being connected to everything and reduced senses of self or ego.
“Our findings move us one step closer to understanding mechanisms underlying how psilocybin works in the brain,” says Frederick Barrett, Ph.D., assistant professor of psychiatry and behavioral sciences at the Johns Hopkins University School of Medicine and a member of the school’s Center for Psychedelic and Consciousness Research. “This will hopefully enable us to better understand why it’s an effective therapy for certain psychiatric disorders, which might help us tailor therapies to help people more.”
Read the whole article at https://www.hopkinsmedicine.org/news/newsroom/news-releases/research-story-tip-psychedelic-drug-psilocybin-tamps-down-brains-ego-center
Natural Products and Safety Issues

National Center for Complementary and Integrative Health sent this bulletin at 12/02/2015 12:18 PM EST
“
Natural products such as herbal medicines or botanicals are often sold as dietary supplements and are readily available to consumers; however, there is a lot we don’t know about the safety of many of these products.
Two of the main safety concerns for dietary supplements are:
—The possibilities of drug interactions—for example, research has shown that St. John’s wort interacts with drugs such as antidepressants in ways that can interfere with their intended effects
—The possibilities of product contamination—supplements have been found to contain hidden prescription drugs or other compounds, particularly in dietary supplements marketed for weight loss, sexual health including erectile dysfunction, and athletic performance or body-building.
As with any treatment, it’s important to consider safety before using complementary health products and practices. Read more at https://nccih.nih.gov/health/safety.“
Additionally…
Dietary Supplements Land Thousands in the ER Each Year
https://www.nlm.nih.gov/medlineplus/news/fullstory_155144.html
Side effects from dietary supplements send more than 20,000 Americans to the emergency room each year, a new government study reveals.
National Survey Shows Different Bacteria on Cellphones and Shoes
From the June 9, 2020 article at UC Davis
Microbes Mostly Harmless, Include Groups Barely Known to Science
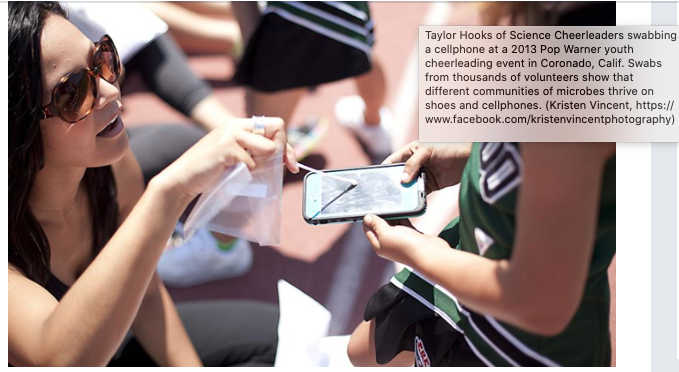
“They found that shoes and cellphones from the same person consistently had distinct communities of microbes. Cellphone microbes reflected those found on people, while shoes carried microbes characteristic of soil. This is consistent with earlier results.
The shoe microbes were also more diverse than those found on a person’s phone.”…
…”Surprisingly, a substantial proportion of the bacteria came from groups that researchers call “microbial dark matter.” These microbes are difficult to grow and study in a lab setting and thus have been compared to invisible “dark matter” that astronomers think makes up much of the universe.
Since they are so difficult to grow in a lab, these dark matter groups have only been discovered as scientists have used genetic sequencing technology to look for microbes in the world around us. Although many of the dark microbial groups come from remote or extreme environments, such as boiling acid springs and nutrient-poor underground aquifers, some have been found in more mundane habitats, such as soil.
“Perhaps we were naïve, but we did not expect to see such a high relative abundance of bacteria from these microbial dark matter groups on these samples,” Eisen said.
A number of these dark microbe groups were found in more than 10 percent of samples, with two groups, Armatimonadetes and Patescibacteria, being found in almost 50 percent of swabs and somewhat more frequently in those from shoes than those from phones. Armatimonadetes is known to be widespread in soil.
“A remarkable fraction of people are traveling around with representatives from these uncultured groups on commonplace objects,” Coil said.”
Are viruses alive? Perhaps we’re asking the wrong question

From the June 8, 2020 article at The Conversation
“The truth is, we don’t fully understand viruses, and we’re still trying to understand life. Some properties of living things are absent from viruses, such as cellular structure, metabolism (the chemical reactions that take place in cells) and homeostasis (keeping a stable internal environment).
This sets viruses apart from life as we currently define it. But there are also properties that viruses share with life. They evolve, for instance, and by infecting a host cell they multiply using the same cellular machinery.”
Read the entire article at https://theconversation.com/are-viruses-alive-perhaps-were-asking-the-wrong-question-139639
Looking for summaries of the best current evidence for healthcare decision making? Cochrane Evidence may have a report on a topic of interest

Cochrane reviews are systematic reviews of primary research of human health care. They are systematic because they review ALL the available journal articles to answer a specific question.. Each systematic review can take up to 2 years and includes at least 2 people.
An example of a question would be
Can antibiotics help in alleviating the symptoms of a sore throat?
Cochrane Reviews do not answer every healthcare question, but they currently have several thousand reviews answering specific questions.
Cochrane Evidence has plain language summaries of the above reviews.
““Cochrane summarizes the findings so people making important decisions – you, your doctor, the people who write medical guidelines – can use unbiased information to make difficult choices without having to first read every study out there…”
Sifting the evidence, The Guardian, 14 September 2016
The Science of Habits: How we make and break them
From the July 1, 2020 article at Medical Express
“Professor Barbara Mullan is the Deputy Head of Curtin University’s School of Psychology. She’s been researching how habits work.
She says the main driver of forming habits is a cue that makes you think of something, which is followed by a reward.
For example, on your drive home, you see a McDonald’s sign (cue) and buy yourself a Happy Meal (reward).
“For a lot of us, we have routines,” Barbara says. “One step which leads to the next step which leads to the next step.”
The good, the bad and the loop
This cycle is called habit loops or habit stacking.
“When we’re trying to get people to form good habits, we often get them to think about something they’re already doing and seeing if they can hook it on to that,” Barbara says.
For example, if you’re trying to remind yourself to take a new supplement, you can put it next to your toothbrush and take it when you brush your teeth.
The reverse is true for breaking bad habits. If you eat lollies when you watch TV, maybe it’s time to stop watching TV for a while.”
Read the entire article at https://medicalxpress.com/news/2020-07-science-habits.html
Someone misunderstanding your SocialMedia post? It could be your Emoji !
Our cultural backgrounds influence how we interpret emojis, U of Toronto study finds (July 22, 2020)
Excerpt
“Working under the supervision of Doug VanderLaan, an assistant professor in the department of psychology, Gao recently published a study in Cyberpsychology, Behavior, and Social Networking that looked at how different cultures interpret emojis – “paralinguistic cues” used to express thoughts and emotions in communication platforms such as email, texts, and social media.

The study built on previous research that shows people from Western cultures pay more attention to in-person cues from the mouth when gauging emotion compared to those from Eastern cultures, who focus more on the eyes.
“Communication using emojis or emoticons may be considered more effective than using words alone because they deliver emotions in a more visually direct manner,” says Gao. “However, emojis are not usually labelled with a fixed meaning and are subject to interpretation, which can vary depending on a person’s cultural background.”
Read the whole summary here
Mouthwashes could reduce the risk of coronavirus transmission
From the August 10 2020 Medicalxpress article
“The use of mouthwashes that are effective against Sars-Cov-2 could…help to reduce the viral load and possibly the risk of coronavirus transmission over the short term. This could be useful, for example, prior to dental treatments. However, mouth rinses are not suitable for treating Covid-19 infections or protecting yourself against catching the virus.”

Go to the PDF, table 1 to see the effectiveness of 8 different mouthwashes available at stores along with the full text of the scientific article.

“Gut Feelings” seem to be science based! As do gut-brain interactions in many diseases and their treatments
From the March 2020 Flinders University news release
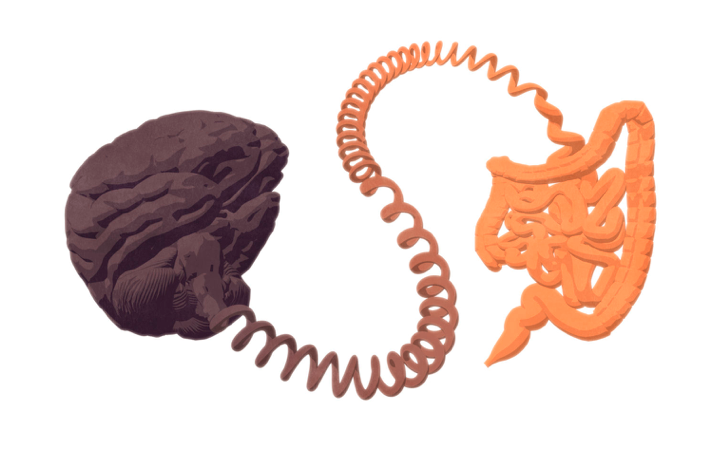
Scientists at Flinders University have, for the first time, identified a specific type of sensory nerve ending in the gut and how these may ‘talk’ to the spinal cord, communicating pain or discomfort to the brain.
This discovery is set to inform the development of new medications to treat problems associated with gut-to-brain communication, paving the way for targeted treatments to mitigate related dysfunction.
While our understanding of the gut’s neurosensory abilities has grown rapidly in recent years, two of the great mysteries have been where and how the different types of sensory nerve endings in the gut lie, and how they are activated.
An important step in answering these questions has been made possible through the development of new techniques by Professor Nick Spencer’s Visceral Neurophysiology laboratory at Flinders University in South Australia.
“We know that many disorders of the brain and gut are associated with each other, so unravelling their connection is critical to developing targeted, efficient treatments for what can be debilitating conditions like irritable bowel syndrome, chronic constipation or ulcerative colitis,” Professor Spencer says.
Professor Spencer’s research revealed an extraordinarily complex array of nerve endings that are located over multiple layers of tissues in the lower colon.
“Our study identified the two classes of neurons involved and their location in a range layers in the colon including muscle and mucus membranes, which are potentially capable of detecting sensory stimuli.”
His research forms one of many studies underway at Flinders University’s five neurogastroenterology laboratories, which are contributing to the growing bank of global knowledge on the gut’s interaction with the brain, including its impact on higher cognitive function.
Why Jigsaw Puzzles Are So Soothing And Addicting Right Now
From the May 27, 2020 Huffington Post article

Short answer..
““While COVID-19 is associated with a lack of control and an unknown end, puzzles offer the opposite,” said Michael Vilensky, a psychologist at Ohio State University’s Wexner Medical Center. “With a puzzle, with enough time and effort, we can control the outcome, know it will end, and experience a sense of relief and accomplishment when it’s finished.””
Read the entire article at https://www.huffpost.com/entry/jigsaw-puzzles-soothing-coronavirus_l_5ecc7d43c5b6d6fc7b7f41b4?ncid=newsltushpmgnews
Getting to the bottom of goosebumps
Harvard scientists find that the same cell types that cause goosebumps are responsible for controlling hair growth
From the July 20, 2020 article at the Harvard Gazette
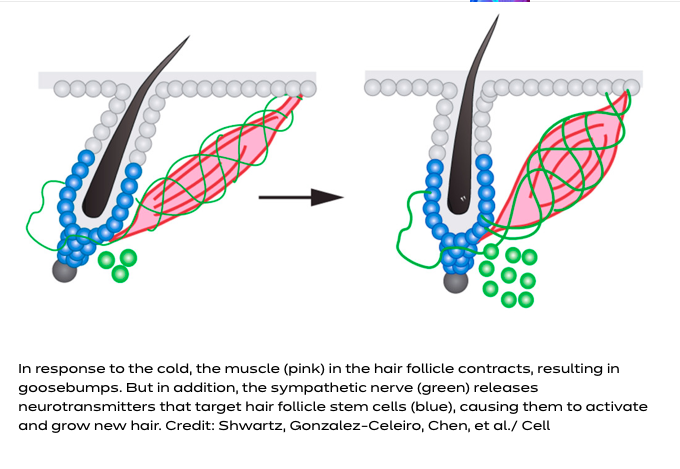
“If you’ve ever wondered why we get goosebumps, you’re in good company — so did Charles Darwin, who mused about them in his writings on evolution. Goosebumps might protect animals with thick fur from the cold, but we humans don’t seem to benefit from the reaction much — so why has it been preserved during evolution all this time?
In a new study, Harvard University scientists have discovered the reason: the cell types that cause goosebumps are also important for regulating the stem cells that regenerate the hair follicle and hair. Underneath the skin, the muscle that contracts to create goosebumps is necessary to bridge the sympathetic nerve’s connection to hair follicle stem cells. The sympathetic nerve reacts to cold by contracting the muscle and causing goosebumps in the short term, and by driving hair follicle stem cell activation and new hair growth over the long term.”
Read the whole summary here
Some ‘Inert’ Drug Ingredients May Be Biologically Active
Comprehensive Laboratory Study Flags Drug Components in Need of More Rigorous Review

The active ingredients in a drug are an extremely small part of the pill, liquid, or injectable, However the inert ingredients in drugs are not just “fillers” so that a pill is easy to handle. They” can be composed of ingredients including preservatives, dyes, antimicrobials and other compounds known as excipients**. These ingredients play critical roles in making sure a drug’s active ingredient is delivered safely and effectively, as well as conferring important qualities like shelf stability and the ability to quickly distinguish pills by color.”
The excipients have been generally been classified by scientists as nontoxic and biologically inactive. Some patients have described side effects from these excipients. A USCF team decided to study if indeed certain excipients are not as biologically inactive as thought. These studies will go a long way in deducing if a person is having side effects from the drug or added ingredients.
So far the team “the researchers have now systematically screened 3,296 excipients contained in the inactive ingredient database, and identified 38 excipient molecules that interact with 134 important human enzymes and receptors.”
Future research will expand on these hypothetical findings and test using animal models.
**Excipients are crucial to drug delivery within the body. Generally, an excipient has no medicinal properties. Its standard purpose is to streamline the manufacture of the drug product and ultimately facilitate physiological absorption of the drug. Excipients might aid in lubricity, flowability, disintegration, taste and may confer some form of antimicrobial function. Selecting the appropriate excipient to support the design of your pharmaceutical formulation is an important step in the drug manufacturing process. From Pharmaceutical Excipients
Read the entire summary here.
How your behaviour on social media could be limiting the quality of your news feeds
From the 16 June 2020 University of Western Australia News Release
Wondering if you are getting good quality and balance information from your news feeds and social media? You might not be alone. Over half the world’s population gets their news from social media. But how reliable are posts on social media? and how to select the more reputable?
First, be careful when you dislike a post or opt to see less of something on a news feed. Even if it seems to be a reputable source.
“Throughout social media, a series of complex algorithms are in place to keep users engaged and visiting social media sites as long as possible. They want the user to have the feeling of ‘you’re right’ so content is tailored to that person.
“This creates an environment of like-minded users who reinforce that person’s opinions rather than providing balanced information.”
So disliking and opting to see less may well result in your missing information from a reputable source.
“The researchers say another possibility would be to make it more difficult for users to share information when an article fails to cite external references. For example, users might be required to click past a pop-up window.
“Another option is what is called boosting, to enhance user competence in the long-term. This could, for instance, mean teaching people to determine the quality of a news item by looking at a set of variables, such as the sources being cited, that determine its likely quality,” he said.”
Related articles
- How to evaluate complementary health approaches in the news (jflahiffwordpress post)
- Misleading information on health social sites (and tips on how to evaluate health/medical information) ((jflahiffwordpress post))
- Evaluating Internet health information (Penn State)
- Evaluating Medical Research Findings and Clinical Trials (Family Caregiver Alliance)
- A Consumer’s Guide to Taking Charge of Health Information (Harvard Center for Risk Alliance)
- Evaluating Health Information on the Internet (National Cancer Institute)
- Quackwatch: Your Guide to Quackery, Health Fraud, and Intelligent Decisions (Stephen Barrett, M.D.)
Better vaccines are in our blood
From the July 13, 2020 article at the Harvard Gazette
Recent studies on mice have shown the red blood cells not only deliver oxygen to our body’s cells. They are also involved in our immune response. Red blood cells deliver antigens (toxins or foreign substances) to special cells in the spleen (antigen-presenting cells) to generate an immune response.
The article goes on to explain why the spleen is an ideal area for this type of immune response. It is one of the few organs where red and white blood cells naturally interact.
This is a good avenue to explore for vaccine development.
Rather than inject only antigens into the blood, the mice studies have shown it is safer and more efficient to inject red blood cells coated with the antigen.
Read the entire news release here.

Study shows humans are optimists for most of life

From the July 13, 2020 Michigan State University news release
“We found that optimism continued to increase throughout young adulthood, seemed to steadily plateau and then decline into older adulthood,” said William Chopik, MSU assistant professor of psychology and lead author. “Even people with fairly bad circumstances, who have had tough things happen in their lives, look to their futures and life ahead and felt optimistic.”
The study included people from ages 16-101. They found that optimism increased from ages 15-60 regardless of good or bad circumstances. Resiliency results from people feeling more in control of their lives as they achieve goals and have successes.
Are viruses alive? Perhaps we’re asking the wrong question

This June 8, 2020 article from The Conversation goes into some depth on how we define life alters how we categorize living versus non-living things.
Viruses have some characteristics of living things as DNA, the ability to change animal and plant DNA, and the ability to evolve. However they do not have a cell structure or a stable internal environment.
The complexity of this question is furthered by posing questions of forms that seem to be life outside of earth. What would be the qualifiers? or the select indicators that life is present?
The article concludes life is a human construct. Nature, evolution, and life exist without human categories. So some theorize that viruses are just on an evolutionary continuum regardless if we call them living or not.
Running shoes may cause injuries – but is going barefoot the fix?

From the April 23, 2020 article in The Conversation
About 100 years ago fashionable shoes started actually changing the shape of the foot! And a recent review concludes “wearing shoes changes the way we run and weakens the foot in a way that can contribute to many common sports injuries.” With ” between 35 and 50% of runners were injured at any one time. ” Most injuries were connected to muscles involved in movement.
Minimalist shoes may reduce injuries along with balance activities. And running barefoot will not guard against all injuries. Age, BMI, previous injuries, and a sedentary lifestyle are all injury factors no matter the shoe.
The article concludes stating “It’s likely that these factors might also make humans less conditioned to move how they did millions of years ago. This suggests a combination of getting more active, walking or running barefoot more often, and other conditioning exercises may help prevent further injuries in the future.”
So, don’t wholly blame the shoe or think a proper shoe alone is the answer!
Taking time to commune with nature increases feelings of connection to it, study shows
Feeling cooped up during this pandemic? Especially if you do not live near a natural area as a park or gardens? Communing with nature, even just by looking out a window with some wildlife, plants, or trees may help. As even growing something from seed inside one’s house may help.

On a related note, some Asian cultures take “nature baths”. That is they go out and walk in woods (clothed!) and just be one with their surroundings, letting go best they can of their everyday concerns.
The link here is to an article describing a study about undergraduate students and how they felt more connected with nature with their studies “in the field”. Many of the results also apply to “the rest of us!”.
Here’s the link–> https://news.nd.edu/news/taking-time-to-commune-with-nature-increases-feelings-of-connection-to-it-study-shows/
Beyond the garnish: Will a new type of produce get the microgreen light?
Microgreens may be the answer. Quicker to grow than baby greens.
Does not have the bitter roots of sprouts.

Great informative yet entertaining tutorial from the Tennessee State Extension Office at https://www.youtube.com/watch?v=QfX59p_E2tw&feature=youtu.be

Accompanying PDF at https://mastergardener.osu.edu/sites/mgv/files/imce/MISC/Resources/microgreens%20handout.pdf
Creative (“traditional”) swearing may help one tolerate pain
Do you want to swear when facing a shot by a healthcare provider? But don’t want to resort to four letter words? Here’s an idea!
https://www.keele.ac.uk/research/researchnews/2020/june/traditional-swearing/tolerate-pain.php
Mind-altering drugs could treat mental disorders
This is an “old” 2016 article, but still under discussion in biomedical circles
https://cen.acs.org/articles/94/i13/Psychedelic-compounds-like-ecstasy-just.html
For anyone interested – Music blog
https://musicadvisor.com/top-benefits-taking-music-lessons-young-adults/
I don’t know much about this blog, to be honest. But am posting upon request.
It seemed interesting, but am posting with disclaimer that I am not associated with this.

Eat better for better mental health, heart health, immune health!
Have mental health, heart health, or immune health issues? Consider altering your diet for better gut microbe colonies. The gut, brain, and immune system are all related and interact.
At this time “There is currently no ‘silver bullet’ probiotic or antibiotic, although certain combinations of probiotics are providing promising research results.”
However, one can most likely foster good bacteria through following a Mediterranean diet.
Read more about this at The American Heart Associations May 28, 2020 article –> https://www.heart.org/en/news/2020/05/28/how-bacteria-in-your-gut-interact-with-the-mind-and-body

What We Know About Possible COVID-19 Treatments And Vaccines So Far

Confused about the current science regarding drugs as hydroxychloroquine and Remesivir? Treatments as convalescence plasma? If Vitamin C works?
The Huffington Post has a good overview of a few treatments and vaccines recently in the news.
Additional Resources
- Mythbusters (World Health Organization)
Coronavirus disease (COVID-19) advice for the public (drinking alcohol, adding pepper to your soup does not work!) - Global Research on Coronavirus Disease (World Health Organization)
Latest scientific findings and knowledge on coronavirus disease - Coronavirus [COVID-19] (US National Institutes on Health)
Includes links to treatment guidelines, news releases (including treatments), and clinical trial information (US and other countries) - Information for Clinicians on Investigational Therapeutics for Patients with COVID-19 (CDC)
Includes link to interim guidelines for the medical management of COVID-19external icon prepared by the COVID-19 Treatment Guidelines Panel (NIIH) - Medwatch (FDA)
Medical product safety reporting program for health professionals, patients and consumers
Trump, the politics of fear and racism: How our brains can be manipulated to tribalism

In situations perceived as dangerous humans have historically tended to trust others in one tribe and authorities of kindred spirits. The downside is politicians seen as authorities (even when they are not) can exploit this trust for their own gain. Politicians will go so far as to dehumanize those outside one’s tribe and portray “the other’ as less worthy and the enemy.
This thought provoking article by The Conversation** can be found at https://theconversation.com/trump-the-politics-of-fear-and-racism-how-our-brains-can-be-manipulated-to-tribalism-139811
**”Academic rigor, journalistic flair
Social psychiatry could stem the rising tide of mental illness
The Conversation is a Web site that bills itself as having “academic rigor, journalistic flair”. It is a great place to go for insightful thoughtful articles on a variety of current event topics.
A June 3 2020 article outlines the history of social psychiatry, ” a preventive approach to mental health that was highly influential in the US after the second world war. It focused on identifying the social factors believed to cause mental illness. These included poverty, inequality and social exclusion. It was also an interdisciplinary approach. Psychiatrists worked closely with social scientists, especially sociologists and anthropologists, to determine the relationship between society and mental illness.”
Historical neighborhoods highlight how poverty, inequality, and social isolation relate to mental illness. In one study “.. patients in the lower classes were more likely to receive invasive, somatic therapies. These included drugs, electroshock therapy and lobotomy. Patients from higher classes were more likely to receive psychoanalysis.”
Prevention was seen as imperative since at least the 1950’s. Indeed, even
President Kennedy was on board.

“In February 1963, Kennedy stressed the role of prevention in a speech to Congress. Americans “must seek out the causes of mental illness and of mental retardation and eradicate them”. In psychiatry, “an ounce of prevention was worth more than a pound of cure”.
By “causes” Kennedy meant “harsh environmental conditions”. But the primary solution he recommended did not address these conditions. Instead, he proposed creating a national network of community mental health centres (CMHCs) to replace the asylum system.”
However, from the late 60’s on social psychiatry was no longer in favor.
Instead there was more reliance on treatment, specifically prescription drugs.
The author ends on a hopeful not. “During the past few years, however, concerns about rising rates of mental illness have put prevention back on the agenda. Although social factors – especially in light of COVID-19 – have been mentioned, there is not enough discussion of policy changes that could make a difference. This was also a problem during the heyday of social psychiatry.”
The author ends with a few radical prevention imperatives. “My research on social psychiatry has convinced me that introducing universal basic income could improve mental health. But other progressive policies, ranging from reducing the working week to ensuring we all have ample time to commune with nature, could also make a difference.”
Experts urge caution in interpreting COVID-19 antibody tests
False positive results are cause for concern
From the May 26, 2020 Washing University School of Medicine in St. Louis News Release

“There are two kinds of COVID-19 tests, and both are critical to controlling this pandemic. Molecular diagnostic tests, first developed in January, detect parts of the COVID-19-causing virus on swabs from people’s noses or throats. Such tests can identify people with active infections, even when they have no symptoms. With widespread and rapid diagnostic testing, people with the virus can be identified quickly and isolated, and anyone who came into contact with them quarantined and tested. Such surveillance and isolation measures can prevent a few cases from mushrooming into an outbreak.”
…
Why are antibody tests for COVID-19 important?
Farnsworth: Antibody testing is really helpful in monitoring how widely a virus has spread within a community. Such testing could help determine how many people have recovered from the virus, even if they never had symptoms. For many viruses, once about 70% of the population is immune – either because they have had a natural infection or, better yet, received a vaccination – infected people are less likely to encounter a susceptible person and give them the virus, so transmission goes down and the epidemic ends. That’s called herd immunity.”
…
If my antibody test is positive, does that mean I’ve had COVID-19 and won’t get it again?
Anderson: A positive test just means your body has produced antibodies in response to a past infection; it doesn’t tell us whether those antibodies will protect you from getting re-infected
…
Can antibody tests decide who can safely go back to work?
Farnsworth: Many people are anxious to get people back to work, but antibody tests may give some people a false sense of security. The problem is that even a highly accurate antibody test like the one we use in our laboratory has false positives and false negative
How should antibody tests be used?
Anderson: There have not been formal guidelines at the national or local levels regarding how exactly these tests should be used. And, in the absence of such guidelines, many people are anxious to get antibody testing. The way I look at such tests is that they’re a tool.…not … the sole source of information for decision-making.
Related Resources
- Coronavirus Disease 2019 – Test for Past Infection (CDC -US Centers for Disease Control and Prevention)
Outlines what results mean (positive or negativbe) and CDC’s work in antinbody testing - How do COVID-19 antibody tests differ from diagnostic tests? (Mayo Clinic)
Outlines 2 types of tests - What COVID-19 Antibody Tests Can and Cannot Tell Us
“Assays that detect prior novel coronavirus infections could reveal the extent of outbreaks. But they may give individuals false security” - COVID-19 (Johns Hopkins University)
Includes- Serology-based tests for COVID-19
This resource serves to provide up to date information on serology tests that are in development or available for use - Molecular-based tests for COVID-19
The diagnostic testing field for COVID-19 is rapidly evolving and improving in quality every day, with many tests focused on diagnosing patients with active viral infections. Read more about molecular-bases tests for COVID-19 here.
- Serology-based tests for COVID-19
Patients with Type 1 Diabetes Spend About $2,500 a Year in Health Care Costs
While insulin comprises a big part of diabetes expenses for children and adults, diabetes-related supplies can cost even more.
From the Jun 1, 2020 University of Michigan Health Lab News Release

“
Adults and children with type 1 diabetes will spend an average of $2,500a year out-of-pocket for health care – but insulin isn’t always the biggest expense – new research suggests.
While out-of-pocket costs for insulin was substantial, it accounted for just 18% of total out-of-pocket expenses for health care, according to the findings in JAMA Internal Medicine.
In fact, insulin accounted for less out-of-pocket spending than diabetes-related supplies, such as insulin pumps, syringes and continuous glucose monitors.”
…
Removing barriers to high-value care
…
“Several states and insurers imposed monthly caps on these [out-of-pocket] costs [for insulin] earlier in 2020. The Centers for Medicare and Medicaid Services just announced that many elderly Medicare beneficiaries will soon pay no more than $35 for a one-month supply of insulin. “
…
More at the news release
Help for paying for diabetes medicine and supplies
- Needymeds – Diabetes Assitance programs
Companies, organizations, nonprofits - Extra Help (sometimes called the Low-Income Subsidy, LIS)
Medicare Part D assistance through the US Social Security Administration - GoodRx
Compare prices
GoodRx collects prices & discounts from over 60,000 U.S. pharmaciesPrint free coupons – Or send coupons to your phone by email or text message - Patient Advocate Foundation – Co-pay Relief
Provides direct financial assistance to qualified patients, assisting them with prescription drug co-payments their insurance requires relative to their diagnosis
Above note working? I will search for you.
Email me at jmflahiff at yahoo